Are antibiotics and alcohol compatible, in which cases is the danger of this combination justified and when is it exaggerated? We answer this question in our article.
Sometimes antibiotics are essential. They are prescribed for various diseases and often this happens completely "at the wrong time": on the eve of a long-awaited holiday or, for example, a corporate party.
Faced with such a situation, some get bored at the festive table, flatly refuse even a glass of wine or a sip of beer, others decide to interrupt the course of antibiotics, being absolutely sure that they cause much less harm to their own body.
Let's make a reservation now: skipping one or two doses of the drug can cancel the effectiveness of treatment, in addition, irregular use of antibiotics will make the pathogen more resistant to its effects and thus only worsen the problem. To defeat the bacteria "hardened" by these experiments, you will need to increase the dose or prescribe a stronger drug.
And what will happen if you drink a glass of wine or a little beer on the background of antibacterial treatment? Probably nothing. According to British scientists, quoted by the Russian Air Force, alcohol in no way affects the action of the most commonly used antibiotics. They are neutral to each other, which means that the unpleasant "side effects" of such a combination should not be expected, of course, if the issue is limited to just one glass of wine and not to mention some drugs that should not be mixed withalcohol in any quantities.
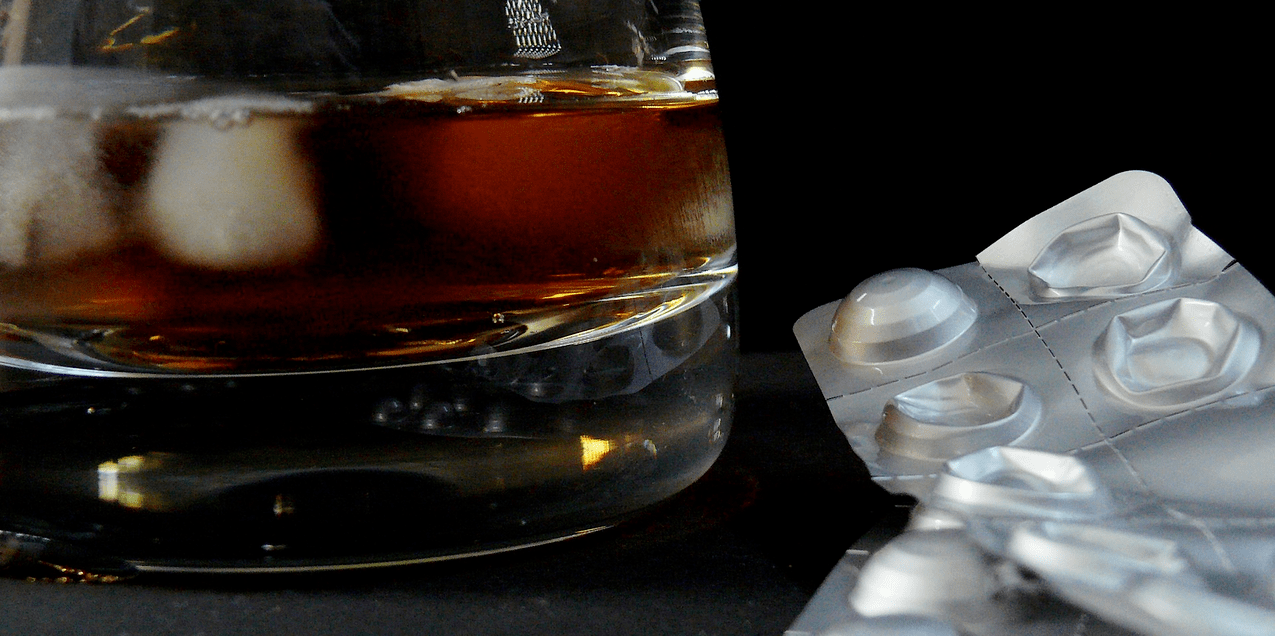
To understand all the risks associated with the concomitant use of any drugs, including antibiotics, with alcohol, you should carefully read the instructions and make sure that this point is not in it.
What antibiotics are best not to combine with alcohol
It is not worth the risk to consume alcohol during treatment with antibiotics that belong to this class, as a number of studies confirm that ethanol weakens their effect.
It is also important to take into account the fact that the substances metronidazole and tinidazole chemically react with alcohol and increase its toxic effect on the liver. However, the data for this result are quite contradictory, but is it worth the risk?
Some members of the cephalosporin group slow down the breakdown of ethanol, thus provoking a disulfiram reaction. These drugs block enzymes that help break down acetaldehyde, which eventually builds up in the body and causes headaches, nausea, tachycardia, shortness of breath, seizures and other unpleasant symptoms.
According to some reports, a similar reaction can be provoked by some bacteriostatic antibiotics, which, however, have not been used as often lately. The combination of alcohol and antifungals is dangerous.

Alcohol and some antibiotics can not only cancel all therapy, but also harm
Prolonged use of antibiotics and alcohol
At the same time, it is important to understand that long-term use of many antibiotics, including erythromycin, rifampicin, tetracyclines, sulfonamides, nitrofurans and lincomycin, accumulates in high concentrations in the bile and over time can lead to toxic liver damage. . As a major detoxification organ, it itself suffers mainly from the side effects of medications. And although phenomena such as cholestatic hepatitis and even fatty infiltration in liver cells are usually temporary, it is still not worth adding an extreme to this important organ, which will have to work with a double load if it is necessary to metabolize both drugs. and alcohol.

Avoiding alcohol is the best option for most medications.
Another argument for avoiding alcohol during antibiotic treatment is the ability of ethanol to cause dehydration and slow down the overall healing process.
With what antibiotics are not yet combined
However, the issue is not limited to giving up alcohol while taking antibiotics. What other medicines a person takes and even what to take with the medicines they take play an important role.
For example, a glass of milk taken with an antibiotic pill or a piece of cottage cheese eaten may negate all the benefits of the drug. Penicillins and tetracyclines, which form stable chelated complexes with calcium, are the worst in combination with dairy products. But it is perfectly acceptable to drink erythromycin with milk.
Antibiotics are not combined with tea, coffee, lemonade, fruit and fruit juices, as well as dishes that contain vinegar.
You should take the antibiotic strictly according to the instructions at regular intervals. If the issue is not limited to taking one drug, it is important to make sure that the drugs do not contradict each other. A qualified doctor, of course, will not prescribe incompatible drugs, but he may not even know that you are currently being treated by another specialist and taking the pills prescribed by him.
For example, the substance cholestyramine and enterosorbent preparations taken concomitantly with antibiotics reduce the absorption of the latter. Taking erythromycin with oral contraceptives may lead to intrahepatic cholestasis, and some antibiotics may reduce the effectiveness of oral contraceptives.
The combination of cephalosporins with thrombolytics is dangerous due to the risk of bleeding, and macrolides and fluoroquinolones may potentiate the toxic effect of theophylline.

The combination of alcohol and a number of drugs can be fatal
What drugs are dangerous to combine with alcohol
Do not combine painkillers, antidepressants, muscle relaxants, antihypertensives, antipsychotics, diuretics, antipyretics, cardiovascular drugs, anticoagulants, painkillers, antihistamines and sleeping pills and oral contraceptives with alcohol. In any case, the side effects will be different and sometimes quite dangerous.
Finally, we note: to avoid problems with antibiotics, read the instructions carefully. And, of course, you don't have to decide to take antibiotics on your own. Your doctor should prescribe them. Self-medication is fraught with serious health problems.
























